Plasminogen deficiency is characterized by the deposition of “woody” membranes, primarily on mucosal surfaces. Despite use of the term “pseudomembrane” to describe these lesions, they are actually true membranes. They are histopathologically characterized as containing abundant subepithelial deposits of paucicellular amorphous eosinophilic hyaline, amyloid-like material which stains positive with periodic acid-Schiff (PAS) and trichrome, negative with Congo red, and is predominantly composed of fibrin.25 These lesions have been described on most mucosal surfaces, but the conjunctiva and gingiva are the most frequently affected.
Ligneous conjunctivitis: Involvement of the conjunctivae has been described in 90% of reported cases and may be bilateral in 65% of cases.16 (See Figures 2a and 2b).
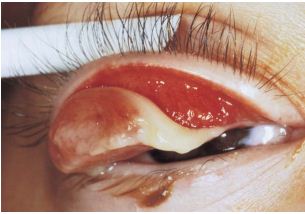
Reprinted from Survey of Ophthalmology, vol 48, Schuster V & Seregard S, Ligneous conjunctivitis, p 369-88, Copyright (2003), with permission from Elsevier.
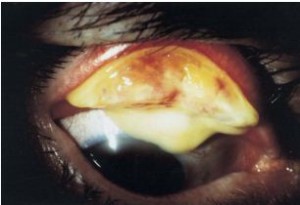
These lesions usually affect the upper eyelid, and initially begin with erythematous conjunctiva and continuous tearing. Pseudomembranes begin as white or red lesions with a woody consistency and replace normal mucosal tissue.1 Approximately one-third of patients have corneal involvement, with a resultant potential for vision loss.1,16 The corneal involvement is secondary to palpebral and bulbar conjunctival lesions with thinning and vascularization leading to ulceration and scaring. Rarely, corneal fibrin deposits2 or large corneal ligneous plaque may occur (Figure 3).26 In mouse models with plasminogen deficiency, corneal ligneous lesions are well documented.27 Although most patients present at a young age (median onset ~1 year),16 there are numerous reports of lesions that do not develop until adulthood. One case series reported an 85 year old individual, while another reported two sisters, aged 71 and 73 years.28,29
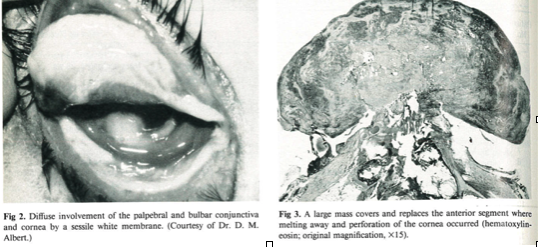
Reprinted from Ophthalmology, vol 94, Hidayat AA, Riddle PJ, Ligneous conjunctivitis: A Clinicopathologic Study of 17 Cases, p 949-59, Copyright (1987), with permission from Elsevier
Ligneous gingivitis (periodontitis): The second most common manifestation is within the oral cavity, with 34-43% of patients expressing ligneous gingivitis (Figure 4).15,16

Reprinted from Survey of Ophthalmology, vol 48, Schuster V & Seregard S, Ligneous conjunctivitis, p 369-88, Copyright (2003), with permission from Elsevier.
Patients may present with only oral lesions or may report other affected areas as well. Gingival lesions are commonly nodular, ulcerated and non-painful with associated hyperplasia.30,31 These lesions often proceed to periodontal destruction, and tooth loss.32
Female reproductive system: Lesions within the female genital tract have been well documented in numerous reports.15,16,33,34,35 Lesions may involve the cervix (ligneous cervicitis), vagina, fallopian tubes, endometrium and ovary. Symptomatic patients may report dyspareunia, vaginal discharge, or dysmenorrhea; in the authors’ experience some patients report the occasional passage of tissue either with or without menses.36 Affected patients typically manifest ligneous lesions in other systems. In one series, 6 of 8 patients were infertile; of the remaining two patients, one was 2 years old, and the fertility of the other was unknown.33
Respiratory tract: Both the upper and lower respiratory tracts have been reported to be affected with ligneous lesions. Laryngeal lesions have led to life-threatening upper airway obstruction.37 Lower respiratory tract masses have been reported to form in the tracheaobronchial tree which can be fatal.1,38
Middle ear involvement: Plasminogen deficiency may be associated with chronic otitis media and pseudomembrane formation around the tympanic membrane or ossicles with the potential for conductive hearing loss.1
Renal collecting system: Involvement of the kidneys and the renal collecting system have been reported.15,39,40
Gastrointestinal tract: Ligneous lesions in the gastrointestinal tract have been reported but appear relatively uncommon. Interestingly, in one case, a patient with a duodenal ulcer had concomitant celiac disease; the association of these two disorders was unclear in terms of the area affected by a ligneous lesion.15,41
Cutaneous involvement: Juvenile colloid milium, a rare skin condition, has been documented in patients with hypoplasminogenemia (Figure 5).1,15,42

Reprinted from Journal of the American Academy of Dermatology, Vol. 49, Oskay T, Erdem C, et al. Juvenile colloid milium associated with conjunctival and gingival involvement, pp 1185-8, 2003, with permission from Elsevier.
These lesions typically occur in sun-exposed areas in childhood, and are characterized by small, translucent, yellow-brown papules.
Central nervous system involvement: Congenital occlusive hydrocephalus has been reported to occur in up to 14% of patients.16 In addition, these patients are at risk for development of a congenital Dandy-Walker malformation with resultant hypoplasia of the cerebellar vermis and cystic dilation of the fourth ventricle.15,16 Unfortunately, the shunts used to drain CSF are prone to occlusion or poor peritoneal absorption, leading some neurosurgeons to recommend ventriculocholecystic shunts.43,44
Thrombophilia: While initial cases of dysplasminogenemia were reported in patients with venous thrombosis, the overall reported rate of thrombotic events in patients with plasminogen deficiency does not appear to be significantly greater than that in the general population. In a series of patients with type I plasminogen deficiency, there were no reported cases of venous thrombosis.15,16 Furthermore, in a large series of patients with type II plasminogen deficiency from Japan, there was no increase in the incidence of venous thrombosis.20
The development of ligneous lesions may be initiated or precipitated by local trauma, inflammation or infection. In ligneous conjunctivitis, upper respiratory infections appear capable of triggering development of these lesions. However, systemic infections, such as urinary tract infections, have also been associated with the development of eye lesions, or lesions in other areas.1 Unfortunately trauma, including surgical excision, appears to stimulate regrowth of pseudomembranes complicating decisions regarding intervention.1